In hyperbilirubinemia, the blood concentration of bilirubin exceeds the normal value. The result is jaundice, since the yellowish substance is deposited in the skin. The treatment depends on the causative disease.
What is hyperbilirubinemia?
The stage of hyperbulirubinemia affects the degree of jaundice present. First of all, a gel coloration of the sclera appears, which can be attributed to the deposits of the increased bilirubin. See AbbreviationFinder for abbreviations related to Hyperbilirubinemia.
Bilirubin corresponds to a yellowish degradation product that comes from the heme part of the red blood pigment hemoglobin. Bilirubin is a bile pigment. Red blood cells have a life span of around 120 days and are broken down within the liver and spleen after this span. After intermediate stages, the red blood pigment becomes bilirubin.
The bilirubin produced daily amounts to around 300 milligrams and comes to around 80 percent from the breakdown processes of the erythrocytes. In the blood, bilirubin is made to bind non-covalently to albumin. The protein-coupled bilirubin corresponds to unconjugated bilirubin. Delta bilirubin is referred to as covalently bound to albumin. In so-called hyperbilirubinemia, the bilirubin concentration in the blood increases to values above 1.1 mg/dl.
If the serum level of the metabolite is elevated, symptoms such as jaundice appear as the bilirubin is deposited in the skin. Depending on the cause and type of bilirubin increase, additional symptoms may appear. Hyperbilirubinemia itself is not a disease in its own right. Rather, it is a symptom of an overarching disease that manifests itself in the form of a breakdown disorder in bilirubin.
In connection with increased total bilirubin, a distinction is made between indirect and direct hyperbilirubinemia. Indirect bilirubin has poor solubility. Better soluble bilirubin, which can be detected as direct bilirubin, is only formed within the liver after biotransformation processes.
Causes
The cause of hyperbilirubinemia is always a disturbance in the breakdown of the waste product. The degradation disorder is considered a symptom of various diseases. Therefore, hyperbilirubinemia can have a variety of causes. For example, indirect hyperbilirubinemia with more than 80 percent of total bilirubin in the form of indirect hyperbilirubin may indicate hemolysis. However, this symptom can also be related to rhabdomyolysis, burns, or neonatal jaundice.
In neonates, elevation is physiological and is considered normal elevation to some extent. Your liver is not yet working fully and therefore breaks down significantly less bilirubin. The causes of indirect hyperbilirubinemia with a small proportion of direct bilirubin and intrahepatic jaundice must be distinguished from the causes just mentioned for hyperbilirubinemia with more than 80 percent of the total bilirubin in the form of indirect hyperbilirubin.
In this context, Gilbert’s disease, Crigler-Najjar syndrome, Dubin-Johnson syndrome or Rotor syndrome may be the cause. The same applies to hepatitis, cirrhosis of the liver or severe intoxication with alcohol, drugs or aflatoxins.
Salmonellosis, cholangitis and leptospirosis must also be considered as causative for this form of hyperbilirubinemia. In the case of hyperbilirubinemia that is directly emphasized with little indirect component and occlusive jaundice, on the other hand, causes such as cholelithiasis, pancreatic carcinoma, bile duct carcinoma or bile duct atresia are sometimes the most common.
Symptoms, Ailments & Signs
Hyperbilirubinemia can manifest itself in clinically different symptoms. In principle, an asymptomatic course is quite possible, for example in the context of diseases such as Meulengracht’s disease. Normally, however, at least the symptom of jaundice appears. The icterus corresponds to jaundice and can be prehepatic, intrahepatic, or posthepatic, depending on the disease.
The stage of hyperbulirubinemia affects the degree of jaundice present. First of all, a gel coloration of the sclera appears, which can be attributed to the deposits of the increased bilirubin. Depending on the cause and type of hyperbilirubinemia, other symptoms and signs may occur, such as nausea and vomiting, abdominal pain, and diarrhea. Some patients suffer from fever and malaise. The symptoms usually appear immediately after the onset of the causative disease and persist for several days to weeks.
Over time, the degradation product is also stored in the rest of the skin and can cause discoloration all over the body. In later stages, deposition occurs in the internal organs and all other tissues of the body. Thus, in the case of late hyperbilirubinemia, the internal tissues of the affected person also turn yellowish.
If the bilirubin crosses the blood-brain barrier in the context of various diseases, developmental disorders can occur as a symptom of the deposits. Storage in vital organs can also be associated with functional losses in the affected organs. Depending on the causative disease, additional disease-specific symptoms may be present, such as itching of the skin.
Diagnosis & course of disease
Bilirubin is determined in the serum. Determination in EDTA blood or heparin whole blood is also possible. When diagnosing hyperbilirubinemia, the doctor compares the total bilirubin with the normal values. If it is more than 1.1 mg/dl, hyperbilirubinemia is present. In addition, the doctor must determine whether the hyperbilirubinemia is direct or indirect.
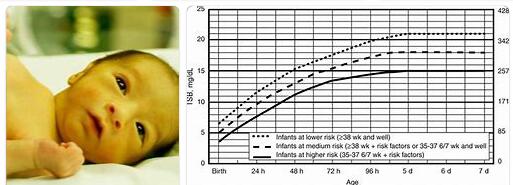
The limit for direct bilirubin is 0.25 mg/dl. For the indirect bilirubin they are 0.8 mg/dl. Different reference ranges apply to infants. The determination of the cause takes place depending on the clinical general picture and usually includes further imaging.
Complications
Hyperbilirubinemia, i.e. an excess of bilirubin above the normal value, occurs primarily in the context of jaundice (icterus). Jaundice can have various causes and complications. Prehepatic jaundice is often caused by increased hemolysis, i.e. the breakdown of red blood cells, which can lead to anemia.
This is characterized by a sharp drop in performance, fatigue and weakness. In hepatic jaundice, the problem is in the liver. In addition to some harmless enzyme defects, hepatitis or cirrhosis of the liver can also be the cause of hyperbilirubinemia. If left untreated, hepatitis can in some cases lead to cirrhosis of the liver, which can subsequently degenerate into liver cancer.
Liver cancer is a dangerous tumor that is fatal if diagnosed too late. The 5-year survival rate is just 10 percent. Posthepatic jaundice is most often due to cholestasis, which is a backlog of bile. The permanent backflow can lead to inflammation and possibly also to bile duct carcinoma.
In the newborn, high bilirubin levels are usually normal and usually subside after a few days. However, if it does not continue to normalize and increase, it can lead to kernicterus. This is severe damage to the central nervous system and can lead to weakness, reluctance to drink and loss of reflexes. If left untreated, the disease can later lead to psychomotor damage and seizures.
When should you go to the doctor?
Hyperbilirubinemia is expressed through jaundice. Like jaundice, hyperbilirubinemia is not a disease in its own right, but a symptom. Hyperbilirubinemia is an underlying condition that interferes with the breakdown of bilirubin from red blood cells. There are many different diseases that can be triggered, for example:
- hepatitis
- liver cirrhosis
- gallstones
- bile duct carcinoma
- bile duct inflammation
- pancreatic cancer
- salmonellosis
- alcohol intoxication
- substance abuse
Hyperbilirubinemia can also occur in neonatal jaundice.
The course of treatment is as diverse as the disease underlying hyperbilirubinemia. It makes sense to see your family doctor first. After initial initial examinations, he decides which other specialists to consult for therapy. Internists, gastroenterologists and oncologists come into question here. There are also a few hereditary disorders that result in hyperbilirubinemia, such as Rotor syndrome, Dubin-Johnson syndrome, and Crigler-Najjar syndrome.
People suffering from a loss of their usual level of performance or general weakness should consult a doctor. If the symptoms persist for a long time or if they increase in intensity, a doctor’s visit is necessary. Tiredness despite getting enough sleep at night, a lack of concentration or attention, and a feeling of illness are all reasons to see a doctor. Discolouration of the skin and in particular a yellow complexion must be examined and treated.
If you have clay-colored stools or dark-colored urine, see a doctor. The changes indicate disorders that need to be investigated and treated. Persistent exhaustion, loss of appetite or a loss of participation in social life should be clarified by a doctor. An unwanted weight loss is to be understood as a warning from the organism. A doctor should be consulted if it develops and causes discomfort.
If everyday obligations or activities can no longer be carried out, a doctor is needed. In the case of disorders of consciousness, the disease is already advanced. An ambulance must be called as soon as loss of consciousness occurs. First aid measures are necessary to ensure the survival of the person concerned. If there is cardiac insufficiency, abnormalities in the circulatory system or circulatory disorders, a doctor must be consulted.
Treatment & Therapy
In many cases, therapy for hyperbilirubinemia is not necessary. In principle, attention is usually paid to the causative primary disease. If this disease corresponds to Rotor or Dubin-Johnson syndrome, for example, therapeutic steps are generally not required.
If hepatitis is present, treatment can range from conservative medication with antiviral drugs to immunosuppressants to liver transplantation. If the cause of hyperbilirubinemia can be resolved, the excess concentration of the substance in the blood will decrease.
If the deposits do not come out of the skin, phototherapy can take place. The bilirubin stored in the skin is converted into a water-soluble substance as part of this phototherapy. This water-soluble substance corresponds to lumirubin, which, thanks to its solubility, can be easily eliminated from the body.
Outlook & Forecast
Hyperbilirubinemia causes jaundice in most people. This can occur for many different reasons, which is why a general prognosis is not possible. If hyperbilirubinemia occurs as a result of alcohol and drug abuse, the drugs must be discontinued and, if necessary, withdrawal carried out.
In other cases, the hyperbilirubinemia occurs due to gallstones or bile duct inflammation, which must be treated by a doctor. The anemia usually leads to a feeling of weakness. The affected person often feels listless and tired and can no longer carry out physical activities. This can lead to underweight and damage to the extremities.
Treatment always focuses on the disease that caused it. If it is hepatitis, a liver transplant can be performed or medication can be administered. As a rule, the hyperbilirubinemia is relatively well limited in this way.
In many cases, however, no treatment is necessary if there is no underlying health-threatening condition that leads to hyperbilirubinemia. In any case, the affected person should still consult the general practitioner so that the cause of the hyperbilirubinemia can be determined.
Prevention
Hyperbilirubinemia can only be prevented to the extent that the causative diseases can be prevented.
Aftercare
In the case of hyperbilirubinemia, those affected usually only have very few measures and options for aftercare. In the case of this disease, a doctor should first and foremost be contacted at an early stage so that the disease can be diagnosed and treated at an early stage. Therefore, a doctor should be consulted at the first signs and symptoms of the disease.
Self-healing cannot occur here, so that treatment by a doctor is always necessary for this disease. Therapy is not required in very few cases. Even without therapy, however, regular examinations of the internal organs by a doctor are very important in order to prevent further complications.
In many cases, patients are dependent on taking medication because of this disease. With this intake, care should be taken to ensure that it is taken correctly and, above all, regularly. If you have any questions or are in doubt, you should always contact a doctor first.
In severe cases, however, organ transplantation is necessary. Bed rest should be observed after such an operation. The person concerned must not exert himself unnecessarily and usually also needs the care and support of the family.
You can do that yourself
Since hyperbilirubinemia occurs as a symptom of a wide range of underlying diseases, no general advice can be given. It is important to strictly follow medical instructions, to take medication regularly and to avoid triggering substances. In the case of prognostically benign causes such as Gilbert’s disease or Rotor syndrome, it is possible to live without any impairment in everyday life.
The greatest influence on the quality of life results from jaundice, ie visible bilirubin deposits in the sclera of the eyes and the epidermis. This is usually a purely cosmetic problem. Not every patient is affected, as this symptom only occurs when the bilirubin concentration in the blood is over 2 µg/dl. In underlying diseases that can be successfully treated, it is completely reversible.
Exposure to light on the skin can make a contribution, albeit a small one, to the degradation of the bilirubin visible on the surface. For this reason, it is advisable not to put make-up on the affected areas or to constantly cover them in the fresh air.
In the case of hyperbilirubinaemia, which can be traced back to substance abuse, self-responsible steps can be taken in addition to therapeutic measures. Visiting relevant self-help groups and participating in abstinence programs can be an important pillar in the treatment that the patient carries out independently of doctors.